Periodontal disease is the main cause of tooth loss in adults and so we take this very seriously at Southgate Dental Care. We have been accepting referrals from our dental colleagues since 1997 and treating advanced gum disease is a big part of what we do.

Dr Stavroula Tsirmpa
Practice Limited to Periodontics
GDC 70601Stavroula graduated from The Dental School of the Aristotelion University of Thessalonica, Greece in 1992. Completed her Master of Science Degree in Periodontics at the University Dental Hospital of Manchester, UK in 1995.
Awarded an EEC scholarship and entered into a clinical and research attachment at the Department of Periodontology at the Royal Dental College, University of Aarhus, Denmark in 1995.
Completed the Certificate in Dental Implantology at the Eastman Dental Institute in 2002.
Joined the Periodontal Department at Queen Mary University of London in 2021 as an Honorary Clinical Research Fellow, Clinical Lecturer in Periodontics and Clinical Supervisor for the Doctorate of Clinical Dentistry in Periodontology (DClinDent).
Research and Development activities focused around laser applications in Periodontics with main focus on periodontal healing and periodontal regeneration
Organiser of Periodontal study clubs within the local dental Community and CPD Lecturing in the field of Periodontics
She has been in Private Practice Limited to Periodontics in Southgate Dental Care, North London and Barkingside Dental Care in Essex since 1997.
She is a member of the British Society of Periodontology, the European Federation of Periodontology and Affeliate Member of the Royal College of Surgeons, Edinburgh.

Dr Shuchi Gupta
Practice Limited to Hygiene
GDC 274645Shuchi joined Southgate Dental care in 2023. Having done BDS and MDS (Periodontics) from India, qualified LDS from Royal College of Surgeons, London (2018)
Shuchi mostly has worked in North London as an Associate.
In India Shuchi has always been academically involved in teaching and research and to continue her passion, is currently working as a Clinical teacher at Kings college, London.
Shuchi has a friendly and caring approach and genuinely enjoys getting to know her patients and building rapport. She strongly believes in maintaining a patient-centred approach to improving oral
health, whilst helping her patients feel at ease in the dental chair. She places great emphasis on good gum health and home care to maintain the existing dental work and prevent further problems.
Outside of Dentistry, Shuchi loves travelling, spending time with family and socialise with friends.

Miss Agnieszka Baran
Hygienist
GDC 296162Aga has graduated as a dental hygienist 2020 from the medical School, Lublin, Poland and joined the team in January 2024.
She is a highly dedicated clinician and is passionate about treating gum disease. She’s a member of the British Society of Dental Hygiene and Therapy (BSDHT).
Her focus is on prevention, patient education and behaviour change - working alongside her patients to achieve optimal oral health.
She provides treatment and maintenance care to the highest standards and tailors her advice for individual patients. Her appointments are relaxed and stress free offering a calm and pleasant experience.
Outside of dentistry she enjoys swimming, cycling and yoga classes.
Periodontal Treatment
Types of Gum Disease
 Untreated gingivitis can advance to periodontitis and eventually lead to tooth loss and other health problems.
Untreated gingivitis can advance to periodontitis and eventually lead to tooth loss and other health problems.
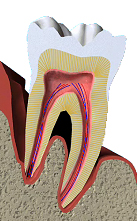
Periodontal (gum) diseases, including gingivitis and periodontitis, are serious infections that, left untreated, can lead to tooth loss. The word periodontal literally means "around the tooth." Periodontal disease is a chronic bacterial infection that affects the gums and bone supporting the teeth. Periodontal disease can affect one tooth or many teeth. It begins when the bacteria in plaque (the sticky, colorless film that constantly forms on your teeth) causes the gums to become inflamed.
 Gingivitis
Gingivitis
Gingivitis is the mildest form of periodontal disease. It causes the gums to become red, swollen, and bleed easily. There is usually little or no discomfort at this stage. Gingivitis is often caused by inadequate oral hygiene. Gingivitis is reversible with professional treatment and good oral home care.
Periodontitis
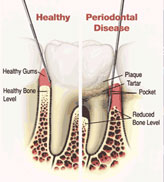
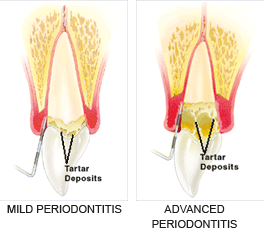
Untreated gingivitis can advance to periodontitis. With time, plaque can spread and grow below the gum line. Toxins produced by the bacteria in plaque irritate the gums. The toxins stimulate a chronic inflammatory response in which the body in essence turns on itself, and the tissues and bone that support the teeth are broken down and destroyed. Gums separate from the teeth, forming pockets (spaces between the teeth and gums) that become infected. As the disease progresses, the pockets deepen and more gum tissue and bone are destroyed. Often, this destructive process has very mild symptoms. Eventually, teeth can become loose and may have to be removed.
There are many forms of periodontitis. The most common ones include the following.
Aggressive periodontitis occurs in patients who are otherwise clinically healthy. Common features include rapid attachment loss and bone destruction and familial aggregation.
Chronic periodontitis results in inflammation within the supporting tissues of the teeth, progressive attachment and bone loss. This is the most frequently occurring form of periodontitis and is characterized by pocket formation and/or recession of the gingiva. It is prevalent in adults, but can occur at any age. Progression of attachment loss usually occurs slowly, but periods of rapid progression can occur.
Periodontitis as a manifestation of systemic diseases often begins at a young age. Systemic conditions such as heart disease, respiratory disease, and diabetes are associated with this form of periodontitis.
Necrotizing periodontal disease is an infection characterized by necrosis of gingival tissues, periodontal ligament and alveolar bone. These lesions are most commonly observed in individuals with systemic conditions such as HIV infection, malnutrition and immunosuppression.
Periodontal Procedures
 Procedures periodontists use to treat gum disease
Procedures periodontists use to treat gum disease
A. Non-Surgical Treatments
B. Periodontal Surgery
Following are some of the procedures that periodontists use to treat patients diagnosed with a periodontal (gum) disease. A periodontist is a dentist who specializes in the prevention, diagnosis and treatment of periodontal disease. Periodontists receive extensive training in these areas, including three additional years of education beyond dental school. Periodontists are familiar with the latest techniques for diagnosing and treating periodontal disease. In addition, they can perform cosmetic periodontal procedures to help you achieve the smile you desire.
A .Non-Surgical Treatments
AAP treatment guidelines stress that periodontal health should be achieved in the least invasive and most cost-effective manner. This is often accomplished through non-surgical periodontal treatment, including scaling and root planning (a careful cleaning of the root surfaces to remove plaque and calculus [tartar] from deep periodontal pockets and to smooth the tooth root to remove bacterial toxins), followed by adjunctive therapy such as local delivery antimicrobials and host modulation, as needed on a case-by-case basis.
Most periodontists would agree that after scaling and root planing, many patients do not require any further active treatment, including surgical therapy. However, the majority of patients will require ongoing maintenance therapy to sustain health. Non-surgical therapy does have its limitations, however, and when it does not achieve periodontal health, surgery may be indicated to restore periodontal anatomy damaged by periodontal diseases and to facilitate oral hygiene practices.
B. Periodontal Surgery
If you're diagnosed with periodontal disease, your periodontist may recommend periodontal surgery. Periodontal surgery is necessary when your periodontist determines that the tissue around your teeth is unhealthy and cannot be repaired with non-surgical treatment. Following are the four types of surgical treatments most commonly prescribed:
 When supporting tissue and bone is destroyed, "pockets" form around the teeth.
When supporting tissue and bone is destroyed, "pockets" form around the teeth.
Your bone and gum tissue should fit snugly around your teeth. When you have periodontal disease, this supporting tissue and bone is destroyed, forming "pockets" around the teeth.
Over time, these pockets become deeper, providing a larger space for bacteria to live. As bacteria develop around the teeth, they can accumulate and advance under the gum tissue. These deep pockets collect even more bacteria, resulting in further bone and tissue loss. Eventually, if too much bone is lost, the teeth will need to be extracted.
 Your periodontist has measured the depth of your pocket(s). A pocket reduction procedure has been recommended because you have pockets that are too deep to clean with daily at-home oral hygiene and a professional care routine.
Your periodontist has measured the depth of your pocket(s). A pocket reduction procedure has been recommended because you have pockets that are too deep to clean with daily at-home oral hygiene and a professional care routine.
During this procedure, your periodontist folds back the gum tissue and removes the disease-causing bacteria before securing the tissue into place. In some cases, irregular surfaces of the damaged bone are smoothed to limit areas where disease-causing bacteria can hide. This allows the gum tissue to better reattach to healthy bone.
What are the benefits of this procedure?
Reducing pocket depth and eliminating existing bacteria are important to prevent damage caused by the progression of periodontal disease and to help you maintain a healthy smile. Eliminating bacteria alone may not be sufficient to prevent disease recurrence. Deeper pockets are more difficult for you and your dental care professional to clean, so it's important for you to reduce them. Reduced pockets and a combination of daily oral hygiene and professional maintenance care increase your chances of keeping your natural teeth – and decrease the chance of serious health problems associated with periodontal disease.
Bone and gum tissue should fit snugly around your teeth
Your bone and gum tissue should fit snugly around your teeth. When you have periodontal disease, this supporting tissue and bone is destroyed and pockets develop. Eventually, if too much bone is lost, the teeth will need to be extracted.
Your periodontist may recommend a regenerative procedure when the bone supporting your teeth has been destroyed. These procedures can reverse some of the damage by regenerating lost bone and tissue.
During this procedure, your periodontist folds back the gum tissue and removes the disease-causing bacteria. Membranes (filters), bone grafts or tissue-stimulating proteins can be used to encourage your body's natural ability to regenerate bone and tissue.
There are many options to enhance support for your teeth and to restore your bone to a healthy level. Your periodontist will discuss your best options with you.
What are the benefits of this procedure?
Eliminating existing bacteria and regenerating bone and tissue helps to reduce pocket depth and repair damage caused by the progression of periodontal disease. With a combination of daily oral hygiene and professional maintenance care, you'll increase the chances of keeping your natural teeth – and decrease the chances of serious health problems associated with periodontal disease.
Your teeth may actually be the proper lengths, but they're covered with too much gum tissue.
Periodontal procedures are available to lay the groundwork for restorative and cosmetic dentistry and/or to improve the esthetics of your gum line.
You may have asked your periodontist about procedures to improve a "gummy" smile because your teeth appear short. Your teeth may actually be the proper lengths, but they're covered with too much gum tissue. To correct this, your periodontist performs crown lengthening.
During this procedure, excess gum and bone tissue is reshaped to expose more of the natural tooth. This can be done to one tooth, to even your gum line, or to several teeth to expose a natural, broad smile.
Your dentist or periodontist may also recommend crown lengthening to make a restorative or cosmetic dental procedure possible. Perhaps your tooth is decayed, broken below the gum line, or has insufficient tooth structure for a restoration, such as a crown or bridge. Crown lengthening adjusts the gum and bone level to expose more of the tooth so it can be restored.
What are the benefits of this procedure?
Whether you have crown lengthening to improve function or esthetics, patients often receive the benefits of both: a beautiful new smile and improved periodontal health – your keys to smiling, eating and speaking with comfort and confidence.
Periodontal procedures are available to stop further dental problems and gum recession
Periodontal procedures are available to stop further dental problems and gum recession, and/or to improve the esthetics of your gum line.
Exposed tooth roots are the result of gum recession. Perhaps you wish to enhance your smile by covering one or more of these roots that make your teeth appear too long. Or, maybe you're not bothered by the appearance of these areas, but you cringe because the exposed roots are sensitive to hot or cold foods and liquids.
Your gums may have receded for a variety of reasons, including aggressive tooth brushing or periodontal disease. You may not be in control of what caused the recession, but prior to treatment your periodontist can help you identify the factors contributing to the problem. Once these contributing factors are controlled, a soft tissue graft procedure will repair the defect and help to prevent additional recession and bone loss.
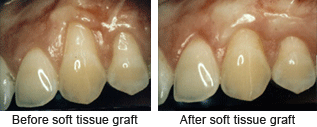 Soft tissue grafts can be used to cover roots or develop gum tissue where absent due to excessive gingival recession. During this procedure, your periodontist takes gum tissue from your palate or another donor source to cover the exposed root. This can be done for one tooth or several teeth to even your gum line and reduce sensitivity.
Soft tissue grafts can be used to cover roots or develop gum tissue where absent due to excessive gingival recession. During this procedure, your periodontist takes gum tissue from your palate or another donor source to cover the exposed root. This can be done for one tooth or several teeth to even your gum line and reduce sensitivity.
What are the benefits of this procedure?
A soft tissue graft can reduce further recession and bone loss. In some cases, it can cover exposed roots to protect them from decay. This may reduce tooth sensitivity and improve aesthetics of your smile. Whether you have a soft tissue graft to improve function or aesthetics, patients often receive the benefits of both: a beautiful new smile and improved periodontal health - your keys to smiling, eating and speaking with comfort and confidence.
What is gum disease
A healthy tooth. Plaque builds up ... ... gum and bone may begin to recede. Sometimes the gum recedes with the bone and sometimes it doesn't. Either way the tooth may become mobile.
|
Gum Disease |
||
| Q | What is gum disease? | |
| A | Gum disease describes swelling, soreness or infection of the tissues supporting the teeth. There are two main forms of gum disease: gingivitis and periodontal disease. | |
| Q | What is gingivitis? | |
| A | Gingivitis means inflammation of the gums. This is when the gums around the teeth become very red and swollen. Often the swollen gums bleed when they are brushed during cleaning. | |
| Q | What is periodontal disease? | |
| A |
|
|
| Q | Am I likely to suffer from gum disease? | |
| A | Probably. Most people suffer from some form of gum disease, and it is the major cause of tooth loss in adults. However, the disease develops very slowly in most people, and it can be slowed down to a rate that should allow you to keep most of your teeth for life. | |
| Q | What is the cause of gum disease? | |
| A | All gum disease is caused by plaque. Plaque is a film of bacteria, which forms on the surface of the teeth and gums every day. Many of the bacteria in plaque are completely harmless, but there are some that have been shown to be the main cause of gum disease. To prevent and treat gum disease, you need to make sure you remove all the plaque from your teeth every day. This is done by brushing and flossing. | |
| Q | What happens if gum disease is not treated? | |
| A | Unfortunately, gum disease progresses painlessly on the whole so that you do notice the damage it is doing. However, the bacteria are sometimes more active and this makes your gums sore. This can lead to gum abscesses, and pus may ooze from around the teeth. Over a number of years, the bone supporting the teeth can be lost. If the disease is left untreated for a long time, treatment can become more difficult. | |
| Q | How do I know if I have gum disease? | |
| A | The first sign is blood on the toothbrush or in the rinsing water when you clean your teeth. Your gums may also bleed when you are eating, leaving a bad taste in your mouth. Your breath may also become unpleasant. | |
| Q | What do I do if I think I have gum disease? | |
| A | The first thing to do is visit your dentist for a thorough check-up of your teeth and gums. The dentist can measure the ‘cuff’ of gum around each tooth to see if there is any sign that periodontal disease has started. X-rays may also be needed to see the amount of bone that has been lost. This assessment is very important, so the correct treatment can be prescribed for you. | |
| Q | What treatments are needed? | |
| A | Your dentist will usually give your teeth a thorough clean. You’ll also be shown how to remove plaque successfully yourself, cleaning all surfaces of your teeth thoroughly and effectively. This may take a number of sessions with the dentist or hygienist. | |
| Q | What else may be needed? | |
| A | Once
your teeth are clean, your dentist may decide to carry out further
cleaning of the roots of the teeth, to make sure that the last pockets
of bacteria are removed. You’ll probably need the treatment area to be numbed before anything is done. Afterwards, you may feel some discomfort for up to 48 hour. |
|
| Q | Once I have had periodontal disease, can I get it again? | |
| A |
|
|